The Kenya Government has been advised to ensure health systems are disease outbreak-resilient and to future-proof against poor service delivery likely to dent poor maternal and child health outcomes.
According to a newly published research report by experts from the African Institute for Development Policy (AFIDEP) in the BMJ Public Health, an international, open access and peer-reviewed journal, analyses in Kenya and Ethiopia highlight the low resilience to disease shocks.
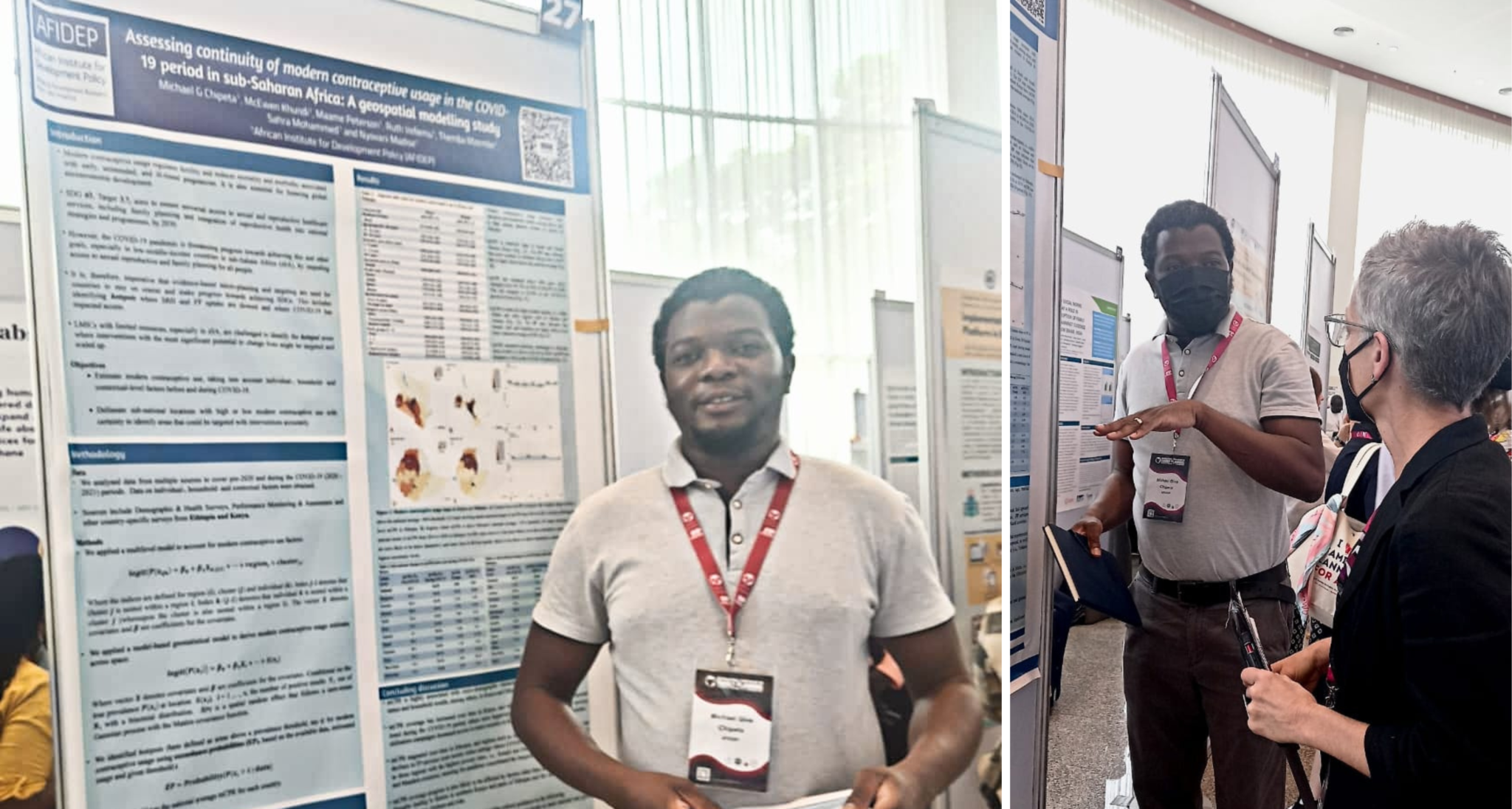
The team, led by Michael Give Chipeta, Senior Research and Policy Analyst at the AFIDEP says that such epidemics as COVID-19 could undermine progress towards sustainable development goals (SDGs) on maternal and child survival.
At the height of COVID-19, for example Kenya imposed strict curfews and lockdown rules to prevent the spread of COVID-19. The Government banned international flights, closed schools, and banned large social gatherings; mass prayer gatherings, large weddings and funerals. In addition to this, the Government issued a 30-day lock down as a mitigation measure to COVID-19 transmission. This was accompanied by a curfew that was initially restricted movement between 7.00 p.m. and 4.00 a.m. but was subsequently extended to 9.00 p.m. to 5.00 a.m.
Read also: 7 Ways to Make the World a Better Place
Despite the directive that expectant mothers be allowed to leave their houses and go to health facilities to access delivery care during emergencies, they however had challenges with transportation to health facilities during the curfew and thus, the preventive measures imposed by the government did not only affect health service delivery but also minimised patient-healthcare workers interaction, especially mothers, for fear of infection by COVID-19.
“Our analyses reveal that the lockdowns and fear of the disease may have reduced access to antenatal care (ANC) and skilled birth attendance (SBA),” said Michael.

He said the team analysed COVID-19’s impact on maternal healthcare usage in the two countries, focusing on subnational levels to identify healthcare disruption hotspots that require targeted interventions and help policymakers prioritise resources to accelerate progress.
The researchers used monthly health management information system (HMIS) data to track changes in healthcare access at subnational levels in Ethiopia and Kenya during the pandemic.
They then compared service usage before and during the pandemic, using interrupted time series and analyses to evaluate the pandemic’s impact on healthcare usage trends. They also performed geospatial mapping of the affected regions to identify hotspots.
The results showed significant changes at subnational levels. ANC declined in several Kenyan counties during the pandemic, with disruptions noted in the two counties.
“Our analysis highlights the low resilience of subnational health systems to shocks, underscoring the need to strengthen healthcare systems,” said researchers.
The team recommend evidence-based research which they note is essential in identifying hotspots and supporting targeted interventions to achieve the SDGs and improve maternal and child health outcomes.
The Novel Coronavirus disease, commonly referred as COVID-19, was declared a public health emergency of international concern on 30th January 2020 and declared a global pandemic on the 11th March 2020 and was declared a public health emergency issue by the then Cabinet Secretary for Health, Mutahi Kagwe on March 15, 2020.
Other team members included Maame Brayie Peterson, Ruth Vellemu, Sahra Mohamed, Themba Mzembe, Chimwemwe Chifungo and Prof Nyovani Janet Madise who also is the head of the Malawi office of the AFIDEP.